Many individuals or couples have questions or concerns about postpartum sexuality. Resuming sexual relations takes time and patience. During the first 6-weeks postpartum, the birth parent’s body is in recovery mode – much more than simply a return to the non-pregnant state! Almost every culture advocates 6 weeks of abstinence for medical or spiritual reasons.
After giving birth, some people have no change in libido and a rare few experience an increased drive. However the majority notice lessening or lack of sexual desire; it’s a normal result of the physical and hormonal changes that accompany birth and post-partum. Most researchers report a return to pre-pregnancy levels of sexual desire, enjoyment, and frequency within a year. The hormones of breastfeeding often lead to suppression of sexual desire. Other factors that play into the temporary decrease in sexual feelings include:
- Lifestyle changes
- Exhaustion or fatigue
- Feeling “touched out” due to constant contact with infant
- Time constrains with duration of sex due to infant needs
- Loss of privacy as a couple
- Individuals in a partnership dealing with new pressures such as how to be a devoted parent or deal with increased financial responsibility
- Many birth-mothers find themselves feeling dependent on their partner partner in new ways – a major mental and emotional adjustment
- Self-image – postpartum people may feel self-conscious of their body and it’s workings
- Relationship satisfaction, which is a predictor of postpartum sexual desire and frequency of intercourse
- Baby blues or postpartum depression
Did you Know?
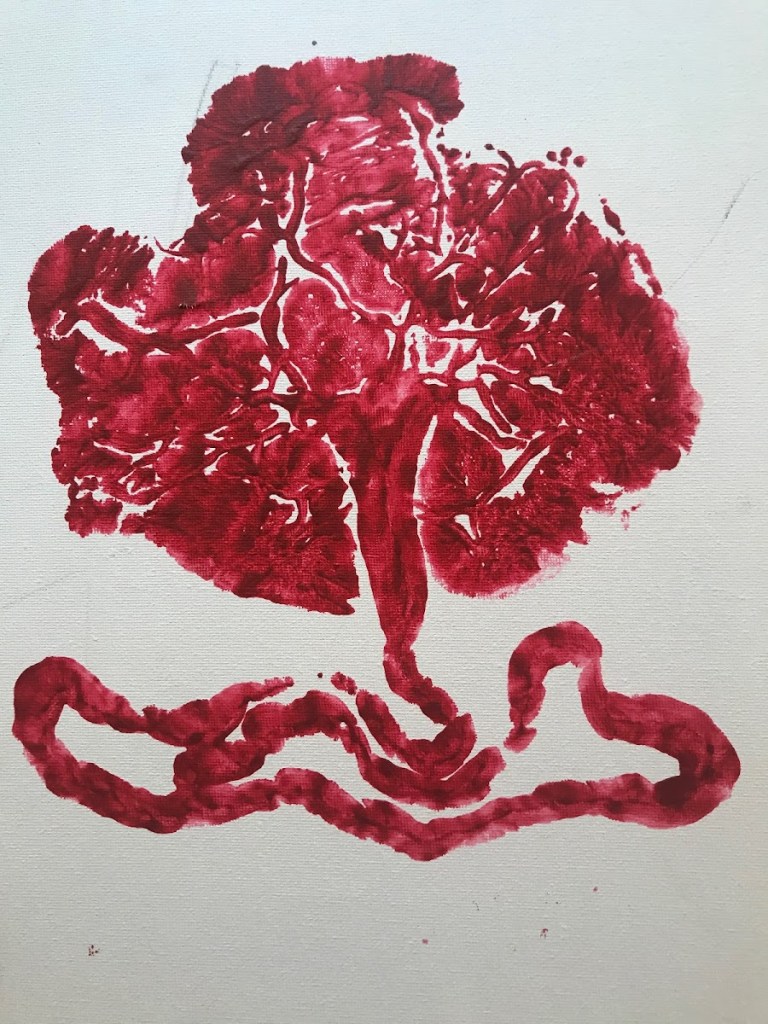
- It takes 6 weeks for the placenta attachment site to heal. During that time there’s actually an open wound in the uterus, at risk for infection or injury.
- The perineum can take 4-8 weeks to heal after incisions or stitches.
- Vaginal secretions are decreased due to postpartum hormone levels.
- Either or both partners may feel shy.
- Jealousy of baby, mother-baby relationship, or partner’s perceived freedom is normal.
- Nipples may be sore or tender. Breasts may leak breast-milk with sexual stimulation.
- Some people feel sexually aroused when their milk lets down.
- It is not normal to have pain with intercourse or using the toilet after 8 weeks postpartum.
The top concerns by both genders at 4 months postpartum include when to resume sexual penetration, birth control, recovery from delivery, and postpartum body image. Have open discussions as a couple.
When to Begin Again…
- To prevent infection or discomfort, wait until whichever is LATEST:
- Postpartum bleeding has fully stopped
- Perineal tears, injuries, sutures heal
- 6 weeks
- **Everyone involved is ready physically, mentally, emotionally**
- Start slowly, especially in cases of traumatic birth
- Stop in case of pain or discomfort
- Patience may be required during the time-period before resuming sexual relations. Try:
- Mutual caring and love
- Cuddling, hugging
- Kissing
- Other sensual, nonsexual contact such as massage
Challenges to Sexuality
- Relationship as both parents transition to parenthood
- Perceived or actual inadequate support and presence of partner
- No time for intimacy, especially if in survival mode
- Difficult or traumatic birth, including Caesarean, can have physical and emotional lingering effects
- Trauma to perineum during birth process
- Religious or cultural beliefs
Other Strategies
- Postpartum support to ensure rest and recovery from pregnancy and birth
- Daily connection and even romance
- If partners find each other attractive or beautiful then tell them, or find something to compliment
- Set aside time for sex when neither of you are tired or anxious e.g. weekly date (day or evening) when someone takes baby for a couple of hours, or a weekly rendezvous while baby sleeps
- Use a lubricant, as it’s normal to be dry or drier than usual, especially if breastfeeding
- Water-soluble are “healthiest” and help with irritation or sensitivity
- Silicone-based last longer and are more slippery than water-soluble
- Avoid petroleum products (Vaseline, baby oil, or mineral oil) as they’re toxic and can dissolve latex condoms or barriers
- Don’t take it personally if if your partner isn’t interested in resuming sexual relations; this will improve with time as hormones and schedules normalize.
Contact Health Care Provider, such as Pelvic Floor Physiotherapist in Case of…
- Pain with penetration or using the toilet beyond 8 weeks that isn’t lessening each week.
- Any questions or concerns regarding sexuality postpartum.
Pelvic Floor Physiotherapy
- Specialists in female pelvic floor care and recovery after birth; also help with prenatal pelvic floor health.
Other Practitioners who can Help
- Painful penetration may be referred to a pelvic floor physiotherapy specialist or gynaecologist.
- Sex therapist in case of non-physical or unidentified origin.
- Couples counselling if relationship is strained.
References
Association of Reproductive Health Professionals. (2006, Sep). Postpartum Counseling – Sexuality and Contraception. Retrieved Sep 2011, from Association of Reproductive Health Professionals: http://www.arhp.org/publications-and-resources/quick-reference-guide-for-clinicians/postpartum-counseling/contraception
Calgary Health Region. (2007). From Here Through Maternity. Calgary: Alberta Health Services.
Davis, E. (1997). Heart & Hands (3rd ed.). Berkeley, CA: Celestial Arts.
Lim, R. (2001). After the Baby’s Birth – A Complete Guide for Postpartum Women (Revised ed.). Toronto: Celestial Arts.
McCabe, M. A. (2002). Psychological Factors and the Sexuality of Pregnant and Postpartum Women. The Journal of Sex Research , 39 (2), 94-103.
Pastore, L. P., Annette Owens MD, P., & Raymond, C. ,. (2007). Postpartum Sexuality Concerns Among First-Time Parents from One U.S. Academic Hospital. The Journal of Sexual Medicine , 4 (1), 115-123.