Good quality nutrition, including adequate protein, is required for the increased metabolic functions that occur during pregnancy. Many midwives and practitioners recommend the Brewer Diet. There’s an overwhelming amount of evidence to support this recommendation. Studies from Harvard find that eating 75 grams of protein daily helps prevent diseases of pregnancy such as pre-eclampsia (Abubakar, A., & al. (2011, Aug)).
In the 1960’s Dr. Tom Brewer worked with a large, high-obstetrical-risk group in California: impoverished ethnic minority teen mothers in their first pregnancy. During the same time in other areas of the USA, this group had up to 35% rates of serious pregnancy diseases, preeclampsia and eclampsia. Dr. Brewer worked with more than 7000 pregnant women over more than 12 years. He asked each woman about her diet and determined that malnutrition was prevalent. All of his clients were required to attend nutritional counselling and were fed good nutrition and adequate protein. The incidence of serious pregnancy illnesses among his patients dropped to 0.5% (Brewer & Brewer-Krebs, 1977)! This is remarkable and well documented but as there was no “control group” (a group who didn’t receive “treatment”, because Dr. Brewer felt it would be unethical to withhold good nutrition from a group of pregnant women), most medical associations don’t consider this scientifically valid research.
The basic Brewer diet recommends a daily minimum of 2600 calories, 80-120 grams protein, salt-to-taste, green veggies, whole grains, fats, and vitamin-rich foods (Jones). The Brewer diet can be easily integrated into general good pregnancy nutrition (see Basic Prenatal Nutrition handout (Evans, 2011)). For example, while the Brewer Diet doesn’t specify types of salt or fat, whole-mineral salts (e.g. Himalayan or Celtic) and high quality omega-3 fats are healthiest. Special needs such as food-sensitivities / allergies, ethical choices or cultural habits can all be incorporated into the Brewer Diet. As usual, ensure you eat 3 meals and 3 snacks daily, including protein at each one.
If you wish to check out the actual “Brewer Diet”, see Dr. Brewer’s Pregnancy Diet Checklists, which include vegan and vegetarian options. Of course you can make substitutions based on your practices and preferences. If you don’t drink milk, sub it for another protein source with calcium. Below is a basic checklist you can use.
Brewer Pregnancy Diet Food Log
The list below is the minimum daily requirements according to Dr. Brewer. You may wish to consult a holistic nutritionist if you have special needs or if you’re having trouble meeting these daily minimums as this requires prompt attention.
Check off a box each time you have a serving. Each food counts as one checkmark on the lists e.g. a glass of milk counts as either “Milk” or “Protein”, but not both. Examples for each category are presented. Modify to fit any special considerations you have, such as vegetarian or a health issue to work around.
DAILY MINIMUMS:
□ □ □ □ □ □ □ □ (8) Calcium source; servings below. Note 125ml = ½ cup
½ cup animal milk, yogurt or sour cream
¼ cup cottage cheese
1 small slice cheese
36 almonds
12 Brazil nuts
1 tbsp raw sesame seeds
1/3 cup cooked bok choy or collard greens
1 cup broccoli, cooked
½ cup kale
2 teaspoons blackstrap molasses
4 oz black olives
1 oz sardines
□ □ □ □ □ □ □ □ (8) Protein; servings below. 1oz = 7g.
Note: See information about fish and mercury on Basic Prenatal Nutrition handout.
1 oz poultry, fish, red-meat, or organs
¼ cup canned salmon or tuna
3 sardines
1 oz cheese: cheddar, Swiss, other hard cheese
¼ cup cottage cheese
1/8 cup brewer’s yeast + 1/4 cup rice
1/8 cup sesame or sunflower seeds + ½ cup cup rice
1/8 cup beans + 1/4 cup whole rice or ½ cup cornmeal (measured before cooking)
□ □ (2) Fresh, dark green vegetables; servings below
1 cup broccoli
1 cup brussels sprouts
½ cup lettuce (preferable romaine)
½ cup endive
½ cup asparagus
½ cup sprouts: bean, alfalfa
2/3 cup greens e.g. collard, turnip, beet, mustard, dandelion, kale, spinach
□ □ □ □ □ (5) Whole grains; servings below
1 slice whole grain bread
1 corn tortilla
½ cup oatmeal, brown rice, quinoa,
1 shredded wheat biscuit
½ cup bran flakes or granola
¼ cup wheat germ
1 waffle or pancake made from whole grain
½ roll, muffin, or bagel made from whole grain
□ □ (2) Vitamin C foods; servings below
½ grapefruit
½ cup grapefruit juice
1 orange
½ cup orange juice
1 large tomato
1 cup tomato juice
½ cantaloupe
1 lemon or lime
½ cup papaya
½ cup strawberries
1 large green pepper
1 large potato, any style
□ □ □ (3) Fats and oils; servings below
1 tbsp butter
¼ avocado
1 tbsp nut-butter
1 tsp algae oil
1 tbsp first/cold-pressed vegan oil – olive, flax, avocado, hemp, coconut
1 tsp cold-pressed fish oil – cod-liver, sardine, mackerel, anchovy, krill
□ (1) Vitamin A foods; servings below
3 apricots
½ cantaloupe
½ cup carrots (1 large)
½ cup pumpkin
½ cup winter squash
1 sweet potato
Salt and other sodium sources—unlimited, to taste
kelp powder–to taste
soy sauce or tamari–to taste
full spectrum natural salt to taste – Himilayan, Celtic i.e. grey or pink salt
Water—unlimited; drink to avoid thirst, not in response to it
Purified water is best – see http://www.angieevans.ca/pdf/Water%20&%20Hydration.pdf
Fresh, home-made juice
Unsweetened herbal tea (see Safe Herbs in Pregnancy handout)
References
Abubakar, A., & al. (2011, Aug). Lipid Profiles and Platelets Counts of Pre-eclamptic women in Selected Rural Areas of Northern Nigeria. WebmedCentral PHYSIOLOGY: http://www.webmedcentral.com/article_view/2121
ACOG. (2002, Jan). Diagnosis and Management of Preeclampsia and Eclampsia; #33. ACOG Practise Bulletin – Clinical Management Guidelines for Obstetrician-Gynecologists: http://mail.ny.acog.org/website/SMIPodcast/DiagnosisMgt.pdf
Brewer, D. T., & Brewer-Krebs, G. (1977). What Every Pregnant Woman Should Know. The Dr. Brewer Pregnancy Diet: http://www.drbrewerpregnancydiet.com/id74.html
Evans, A. (2011). Basic Prenatal Nutrition. Canmore.
Frye, A. (2007). Understanding Diagnostic Tests in the Childbearing Year, 7th Ed. Portland, OR: Labrys Press.
good nutrition… for healthier moms and babies. (n.d.). BlueRibbonBaby.org: http://www.blueribbonbaby.org/
Haas, A. (1995). Preventing Preeclamsia, PIH, Toxemai and HELLP by Good Nutrition. Midwifery Today .
Jones, J. M. (n.d.). The Dr. Brewer Pregnancy Diet: http://www.drbrewerpregnancydiet.com/
Maine, D. (2000). Role of nutrition in the prevention of toxemia. The American Journal of Clinical Nutrition , 72 (1), 298-300.
NICE. (2010, Aug). NICE clinical guideline 107: Hypertension in pregnancy. NHS – National Institute for Health and Clinical Excellence: http://www.nice.org.uk/nicemedia/live/13098/50418/50418.pdf



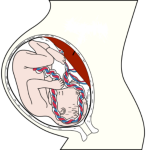 Baby in optimal position: head down and flexed, back out.
Baby in optimal position: head down and flexed, back out.








