In spite of a mountain of evidence to support the benefits of leaving the newborn cord intact, immediate cord clamping is still routine care in many hospitals. At the time of birth, up to 40% of the newborn’s blood is in the placenta. Leaving the cord intact for at least 1-3 minutes ensures the baby gets the majority of their blood, including red blood cells, iron and blood volume. Iron deficiency can lead to anemia and neurodevelopmental delays. Adequate oxygenated blood is required to help the baby adapt to life outside the womb, including how their blood circulates and how well they breathe in the first minutes.
The Cochrane Review, considered the highest standard globally in evidence-based health care information, contains countless articles on the benefits of delayed cord clamping. There are indisputable improved outcomes in babies born at full term and prematurely.
The placental blood normally belongs to the infant, and his/her failure to get this blood is equivalent to submitting the newborn to a severe hemorrhage at birth. (DeMarsh, 1941)
Yes, we’ve known since 1941! Changing practise takes a long time indeed.
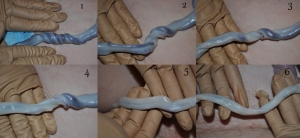 Intact cord – birth to 15minutes (Elphanie, 2011)
Intact cord – birth to 15minutes (Elphanie, 2011)
Benefits of Optimal Cord Care
Benefits and positive effects last well past the newborn period!
- 40% more blood volume.
- 45-50% increased levels of red blood cell counts and blood iron levels.
- Up to 45,000 stem cells (compared to 0 with immediate clamping). Stem cells provide therapeutic benefits to the baby, even into adulthood.
- Protection from anaemia and iron deficiency for at least 6 months.
- Better neurological development.
- More stable vital signs; they thrive better.
- Preemies are less likely to require blood transfusion, ventilation and oxygen therapy.
- Significantly lower rates and less severity of common, major newborn health issues in preemies.
What About Jaundice?
Prevention of jaundice is often cited as the reason to rush the cord clamping. Leaving the umbilical cord intact does not lead to “pathological jaundice” (the kind that makes babies sick). The naturally occurring “physiological newborn jaundice” has no clinical significance, meaning it does not harm the baby. It is normal for healthy newborns to have some jaundice around day 2-3.
Objections by your medical care provider?
The World Health Organization recommends the cord stay intact for 1-3 minutes after the birth (WHO, 2014).
The Society of Obstetricians and Gynaecologist of Canada (SOGC, 2021) states: Delaying cord clamping for at least 1-3 minutes after delivery allows more of the baby’s blood to return from the placenta into the baby and is usually advantageous for the baby. Delayed cord clamping (anytime beyond 60 seconds after delivery) has benefits to the baby. This is because delayed cord clamping allows more blood to transfer from the placenta to the infant, which increases the baby’s red blood cells and iron stores, and reduces the risk of anemia.
“The WHO and the SOGC recommend that cord clamping should be delayed by ≥60 seconds in babies who do not require resuscitation, irrespective of the mode of delivery.” (Armson, Allan, Casper; 2018).
The practise guidelines of the Royal College of Obstetricians and Gynaecologists in the United Kingdom are to leave the cord intact for at least 1 minute and up to 5 minutes, and to leave it for longer than 5 minutes if requested by the birth mother (NICE, 2016).
Even the American College of Obstetricians and Gynecologists (ACOG) recommends a delay in umbilical cord clamping for at least 30-60 seconds after birth, “given the numerous benefits to most newborns” (ACOG, 2017). It’s not enough but is a big step forward for ACOG, notoriously interventionist.
What About Stem-Cell or Cord-Blood Banking?
Delayed cord clamping can not be done with cord-blood banking. Here’s some food for thought…
In British Columbia the maximum allowable blood draw volume in newborns is 5% of their total blood volume in a 30-day period. Other jurisdictions have the same guidelines. For example, a 7# baby has approximately 275ml of blood. Medical testing allows just under 14ml of that baby’s blood to be drawn and tested, total, in one month.
The volume collected for cord-blood banking is normally 60-90 ml or more! That’s more than 5x the allowable monthly blood draws, taken all at once in the first seconds of the baby’s life.
Have you ever noticed all the pamphlets for cord blood banking companies at your Obstetricians’ office? Have you ever seen any information on the benefits of optimal or delayed cord clamping beside those pamphlets? “All pregnant women should be provided with unbiased information about umbilical cord blood banking options.” Society of Obstetricians and Gynaecologist of Canada (SOGC).
Did you know whoever collects the cord blood (usually a doctor or midwife) gets paid to do so by the blood banking company?
Did you know cord-blood banking is a very expensive endeavor? You’ll pay for the kit, possibly for the courier, and then pay every year to store the stem cells.
The Geeky Stuff: Basic Newborn, Placenta & Umbilical Cord Information
- The placenta is nature’s neonatal life-support system.
- The placenta will deliver oxygen to the baby until their newborn lungs transition to breathing air (30 to 90 seconds in a full-term infant).
- Placental transfusion (blood moving from placenta to baby’s body) rate: 50% in 1 minute; nearly 100% over the next 2 to 5 minutes.
- “Delayed” in research ranges from 30sec – 3min, depending on the researcher and study.
- Newborns cope well with lack of oxygen for up to 20 minutes (only if the cord is intact) but low blood volume can quickly have catastrophic outcomes.
- For comparison of the fact that up to 40% of the newborn’s blood is in the placenta, adults may go into shock and receive blood transfusions at 15 to 30% blood-loss.
References
ACOG American College of Obstetricians and Gynecologists. (2017). Delayed Umbilical Cord Clamping After Birth. Obstet Gynecol 2017;129:e5–10. http://www.acog.org/Resources-And-Publications/Committee-Opinions/Committee-on-Obstetric-Practice/Delayed-Umbilical-Cord-Clamping-After-Birth
Armson, B.A., Allan, D.S., Casper, R.F. (2018). Delayed Cord Clamping and Umbilical Cord Blood Collection. Journal of Obstetrics and Gynaecology Canada, 40 (2), 155.
Asfour, V., & Bewley, S. (2011). Cord clamping practice could affect the ratio of placental weight to birthweight and perinatal outcomes. BJOG: An International Journal of Obstetrics & Gynaecology., 118 (12), 1539-40.
Chaparro, C. M., Neufeld, L. M., Alavez, G. T., Cedillo, R., & Dewey, K. G. (2006). Effect of timing of umbilical cord clamping on iron status in Mexican infants: a randomised controlled trial. The Lancet, 367 (9527), 1997-2004.
CRYO-CELL International Inc. (2019). Cord blood collection instructions. Florida.
De Marsh, Q. B., et al. (1941).”The Effect of Depriving the Infant of its Placental Blood.” Journal of the American Medical Association (J.A.M.A.),
Fogelson, D. N. (2011). Delayed cord clamping grand rounds. USC School of Medicine, A.P. Dept. Obstetrics and Gynecology. South Carolina: Palmetto Health Grand Rounds.
Frye, A. (2004). Holistic midwifery, vol 2, Care during labour and birth. Portland: Labrys.
Greene, A. (2008). How much blood is too much guideline. Retrieved from Dr Greene: http://www.drgreene.com/article/how-much-blood-too-much-guideline.
McAdams, R.M. (2014). Obstet Gynecol. 123(3):549-52. doi: 10.1097/AOG.0000000000000122.
Mercer, J. S., Vohr, B. R., McGrath, M. M., Padbury, J. F., Wallach, M., & Oh, W. (2006). Delayed cord clamping in very preterm infants reduces the incidence of intraventricular hemmorhage and late onset sepsis; a randomized, controlled trial. Pediatrics, 117 (4), 1235-1242.
NICE National Institute for Health and Care Excellence (UK). (2016). Clinical guideline [CG190] Intrapartum care for healthy women and babies. Pub Dec 2014, revised/updated Nov 2016. https://www.nice.org.uk/guidance/cg190/
Reed, R. (2011). Cord blood collection: confessions of a vampire-midwife. Retrieved from Midwife Thinking: http://midwifethinking.com/2011/02/10/cord-blood-collection-confessions-of-a-vampire-midwife/
Richmond, S., & Wyllie, J. (2010). European resuscitation council guidelines for resuscitation 2010. Section 7. Resuscitation of babies at birth. J. Resuscitation , 1389-1399.
SOGC. (2021). Delayed Cord Clamping. Society of Obstetricians and Gynaecologist of Canada. https://www.pregnancyinfo.ca/birth/delivery/delayed-cord-clamping/
Tolosa, J. N., Park, D.-H., Eve, D. J., Klasko, S. K., Borlongan, C. V., & Sanberg, P. R. (2010). Mankind’s first natural stem cell transplant. J. Cell. Mol. Med. , 14 (3), 488-95.
University of British Columbia – Children’s & Women’s Health Centre of British Columbia. (2013). Pediatric Blood Draw Guidance. Version 3.2.
Usher, R., Shephard, M., & Lind, J. (1963). The Blood Volume of the Newborn Infant and Placental Transfusion. Acta Paediatrica – Nurturing the Child , 52 (5), 497-512.
WHO. (2014). Guideline: Delayed Umbilical Cord Clamping – for improved maternal and infant health and nutrition. Geneva: World Health Organization.
